“Those who go to urban hospitals have been described as ‘bypassing’ rural hospitals,” according to a July 2014 report by the CDC’s National Center for Health Statistics.
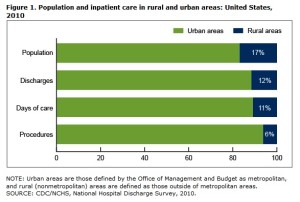
The report by M.J. Hall and M.F. Owings, based on findings from the CDC’s National Hospital Discharge Survey, indicates that 40% of rural (non-metro) residents who were hospitalized in 2010 went to urban hospitals while 60% were admitted to rural hospitals. An April 2014 report by the same authors noted that while 17% of the U.S. population lived in nonmetro areas, 12% of hospitalizations were in rural hospitals.
Residents and hospital staff are often concerned when they know that many potential patients opt for care in larger cities. They know that rural hospitals must be used if they are to remain viable and available for the patients who need them. The people who depend on rural hospitals tend to have fewer resources than other rural residents.
According to the July report, people admitted to rural hospitals tended to be older and were more likely to have Medicare. While 80% of rural residents in urban hospitals received routine discharges, only 63% leaving from rural hospitals received routine discharges. Of course, the fact that rural patients were older is likely to have affected this statistic. In the April report, the CDC reported that 14% of rural inpatients were discharged to a long-term care facility.
Patients want the best care possible, and many perceive that such care is available in cities. Rural doctors, hospitals, and clinics strive to provide the best care possible as well, but rural facilities often lack the latest technology and conveniences. Because they see fewer cases, rural providers may have less experience with any given condition.
Although specialists may travel to rural locations on select days or participate in telemedicine, they may not have the facilities or support staff to complete some procedures or manage intensive cancer therapies. According to the July report, 74% of rural residents who travelled to urban areas for hospitalization received surgical or non-surgical procedures, compared to only 38% of patients in rural hospitals. The April 2014 report also notes that urban hospitals are significantly more likely to have cancer patients.
What is The Role of Rural in healthcare? The answer is hotly debated, as those familiar with rural health systems or even those who read rural newspapers can attest. For some, rural hospitals and clinics are a key component of rural quality of life and the rural economy. The National Center for Rural Health Works has noted that seeing a non-local doctor increases the likelihood of picking up a prescription out of town as well, “bypassing” (in the words of the CDC report) two potential transactions in the rural community. Doctors, nurses, and staff are also likely to live in and/or spend their earning in the local community, creating a multiplier effect. And, many people point out that healthcare is critical to attracting new residents, particularly retirees. For example, GO TEXAN Certified Retirement Communities must provide evidence of the availability of healthcare and related services. The poor, the elderly, and those with the least resources and options need access to care.
On the other hand, people want the best care they can afford, which may come from specialists and even specialty hospitals in urban areas. Many rural areas are within a few hours’ drive of a metropolitan area. Many people contend that rural hospitals with limited tax bases should focus resources on triage and treatment of conditions they are best equipped to treat well, such as acute conditions and those associated with aging. The April CDC report noted that rural hospitals have a relatively large share of hospitalizations for bronchitis and pneumonia. Designation as a critical access hospital (CAH) may provide more flexible staffing requirements and help attract physicians, and cost-based Medicare reimbursement may improve a hospital’s financial performance. However, each community must evaluate whether a CAH is financially advantageous and meets the needs of its residents.
Rural Health Works provides tools to calculate local need for a primary care physician or specialist. Their calculations are based on CDC-NCHS research detailing visits for various conditions or specialties for both males and females in several age categories. For example, the average 65- to 74-year-old male visits a primary care physician 5.5 times per year but only visits a general surgeon about once every five years. Many communities or even counties are unable to support a full-time general surgeon or physicians with various specialties, but working with other regional hospitals or healthcare systems may facilitate access to specialists. Regional collaboration can be between neighboring rural hospitals or between rural and urban systems.
Resources:
Hall, M.J., and M.F. Owings. 2014a. Rural and Urban Hospitals’ Role in Providing Inpatient Care, 2010. NCHS Data Brief 147, Centers for Disease Control, National Center for Health Statistics, Atlanta, GA, April. http://www.cdc.gov/nchs/data/databriefs/db147.htm#fig2
Hall, M.J., and M.F. Owings. 2014b. Rural Residents Who Are Hospitalized in Rural and Urban Hospitals: United States, 2010. NCHS Data Brief 159, Centers for Disease Control, National Center for Health Statistics, Atlanta, GA, July. http://www.cdc.gov/nchs/data/databriefs/db159.htm
National Center for Rural Health Works. http://ruralhealthworks.org/
–Eilrich, F.C., J.C. Sprague, B.C. Whitacre, L. Brooks, G.A. Doeksen, C.F. St. Clair. 2010. The Economic Impact of a Rural General Surgeon and Model for Forecasting Need. National Center for Rural Health Works, Ce Oklahoma State University, September. http://ruralhealthworks.org/needsassessment/
–Eilrich, F.C., G.A. Doeksen, C.F. St. Clair. 2009 .Starting a Practice: Critical Economic Decisions Associated with Locating and Operating a Rural Primary Care Physician Practice. National Center for Rural Health Works, Ce Oklahoma State University, March. http://ruralhealthworks.org/profitability/
GO TEXAN Certified Retirement Communities. http://www.retireintexas.org/Home/CertifiedRetirementCommunities.aspx